Healthwatch 100: parental mental health

For Mental Health Week 2022 we opened a Healthwatch 100 survey on parental mental health between May and August 2022. We wanted to find out more about the kind of support those struggling could access, and how easy they found it to do so. Our results show that there is support available from a variety of sources. However, there is significant room for improvement, and many local people felt that they did not get the help they needed.
Healthwatch Trafford had looked at the issue of maternal mental health in 2019, and this report builds on some of the work already done. The project from 2019 fed into a wider piece by Healthwatch England, and can be found at the link below:
At that time, it was found that across England there were people facing mental health issues around the time of their child’s birth.
Although most respondents identified as ‘female’, we still received several answers from people who identified as ‘male’ or ‘other’. This illustrates the way mental health problems can affect both the person giving birth as well as their partner.
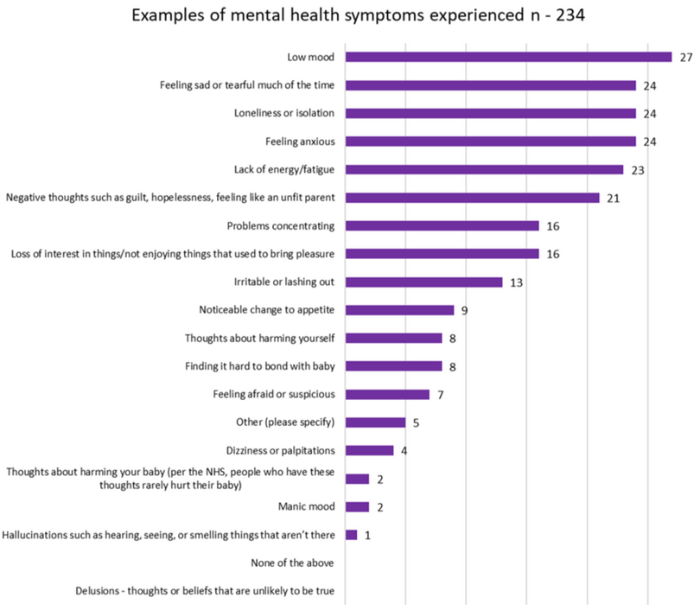
People told us they experienced a wide range of symptoms, both mental and physical. Most respondents experienced low mood, negative thoughts, and fatigue.
What people told us
- Most of the stories we heard happened over 12 months ago.
- Most people who responded did experience mental health issues both before and after the birth of their child.
- Most people’s symptoms lasted a long time, with some still ongoing.
- Most people experienced feelings of sadness, low mood, and anxiety.
- Two thirds of people reached out for support with their symptoms.
- Most people contacted their GP for help, but some other sources people reached out to included counsellors, friends and family, mental health services, midwives, and the hospital.
- Two thirds of people got some of the help they needed; less than half said they had received all they needed.
- Language barriers, support for partners, and preventative support were also flagged as important issues.
- People wanted clear communication about what would happen to them at every stage of pregnancy. Post-natal support in the community was also important.
- When we asked what went well, people praised the support from their GPs, as well as health visitors.
Highlights from the responses
We asked if people sought help and support, and 67% of survey respondents said they did.
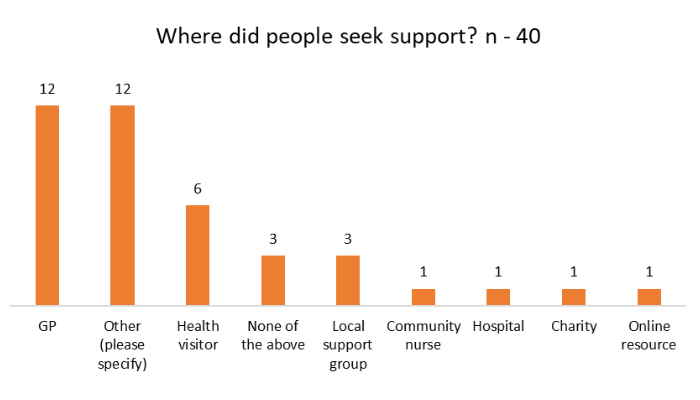
Most people turned to their GP or ‘other’, which people told us included friends and family, midwives, and other mental health services.
While many people reached out, not everyone felt they had been properly supported. Over half the people we heard from felt that support took too long or not the right amount of time to access and only 11% felt they received all the help they needed.
Here are selected comments from Trafford residents:
- “ The problem I had … was that I didn't know what was going on and therefore I wasn't retaining information to even think about asking for help. … Some of the mental health would be helped by being prepared better physically and practically. I thought that the antenatal group I went to would go through the practical stuff for after the birth, but it didn't. … Someone said that they would come round the wards to check on breast feeding, but they didn't … I thought I was breast feeding but it turned out I wasn't, but I didn't know … I had to walk to get my own meals when I could hardly stand in hospital. … Being asked a yes and no question, is not a great way of handling someone who has just been drugged up. We have no clue what is happening.”
- “I never sought any support for the trauma, anger and anxiety that the experienced caused because I was afraid that someone would decide I was unfit to parent my child.”
- “I applied for counselling but it was a long process and I was turned down, despite having felt suicidal. Response [times] for counselling need to be shorter.”
Our recommendations
- A third of respondents did not seek help, saying they either did not know how or felt very alone. We recommend that clear and simple information about sources of help is made available throughout the parental journey, from pre- to post-natal.
- One respondent commented that one of their twins died before birth and they were given no support. This understandable made any mental health issues much worse. People need signposting to specific services like bereavement counselling.
- Another person told us they had to ask for a health visitor before they got help with their mental health. The pathway to support services should be clearer, and there should be analysis throughout pre- and post-natal periods to identify issues and assign appropriate support (including community services where needed).
- The previous work by Healthwatch England recommended the NICE guidelines on care around pregnancy be followed. This remains a goal.
- There needs to be better communication to patients overall. The comments we received suggest that well- handled advice and support can make all the difference. Likewise, one negative interaction can make things worse for parents’ mental health.
More research
In October 2022, Healthwatch England opened a survey calling for more experiences around maternal mental health which can be found by clicking the link below:
Downloads
Download the full report including statistics below. If you require this in an alternative format, please get in touch.
